Disease prevention and control are essential components of public health management, aimed at reducing the burden of illness in populations, improving quality of life, and promoting health equity. Effective strategies focus on anticipating health threats, managing existing health conditions, and preventing future outbreaks. Here’s a detailed look into disease prevention and control in the context of public health management.
1. Levels of Disease Prevention
Public health approaches disease prevention through three levels: primary, secondary, and tertiary.

- Primary Prevention: This level focuses on preventing the onset of disease before it occurs. Efforts include vaccinations, health education campaigns on healthy lifestyles, safe drinking water, and sanitation practices. For instance, vaccination programs for polio, influenza, and hepatitis are crucial in primary prevention.
- Secondary Prevention: Secondary prevention involves the early detection of diseases and interventions to halt or slow disease progression. Screening programs for conditions like cancer, diabetes, and hypertension are examples. Early detection ensures timely treatment, reducing the severity of diseases.
- Tertiary Prevention: This level aims to reduce the impact of long-term diseases by helping people manage their conditions. Rehabilitation programs, chronic disease management, and support groups are all part of tertiary prevention. It focuses on minimizing complications and improving the quality of life for those already affected.
2. Control of Communicable Diseases
Controlling communicable diseases is a critical focus in public health management, involving interventions that target pathogens and transmission routes. Key strategies include:
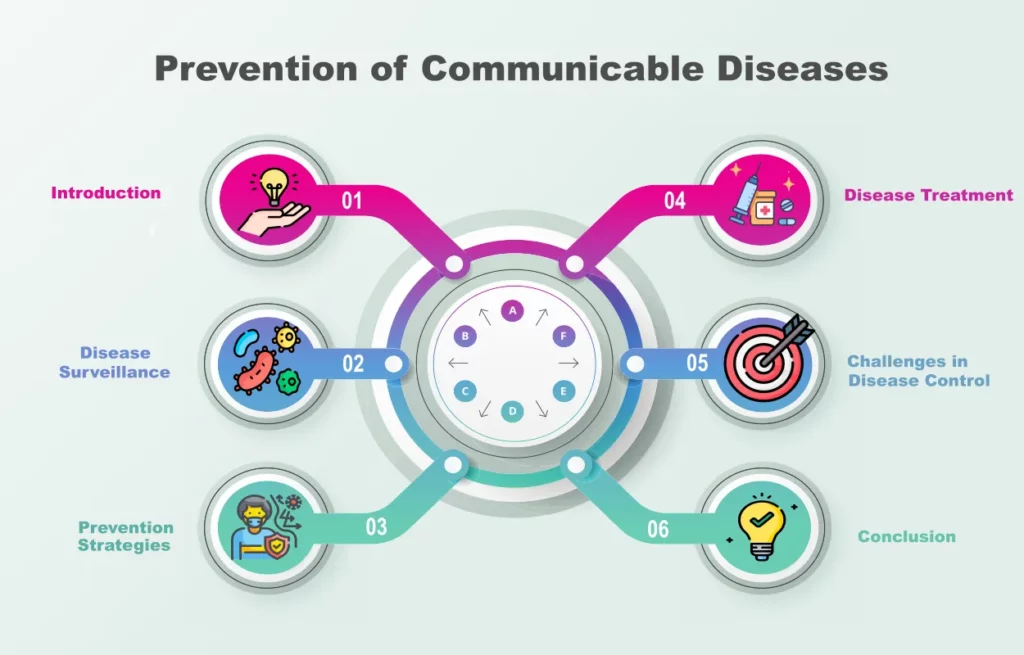
- Surveillance Systems: Continuous monitoring of disease patterns helps identify outbreaks early. Public health agencies rely on data collection and analysis to respond quickly to emerging diseases like COVID-19, Zika virus, and Ebola.
- Vaccination Programs: Widespread immunization campaigns are a cornerstone of preventing the spread of contagious diseases. Vaccines have played a crucial role in eradicating smallpox and controlling measles, rubella, and diphtheria.
- Quarantine and Isolation: During outbreaks, isolating infected individuals and quarantining those exposed is vital for preventing disease transmission. This was a significant strategy during the COVID-19 pandemic.
- Health Education: Informing communities about hygiene practices, safe sexual behaviors, and proper nutrition helps reduce the spread of communicable diseases. Public health campaigns promote awareness about hand washing, safe food handling, and the use of insect repellent to prevent diseases like malaria and dengue.
3. Control of Non-Communicable Diseases (NCDs)
The global burden of non-communicable diseases such as cardiovascular diseases, cancer, diabetes, and chronic respiratory diseases is rapidly increasing. Public health management must address this challenge through:
- Health Promotion: Programs that promote physical activity, healthy eating, and smoking cessation are vital in preventing NCDs. Public health campaigns encourage behavior change to reduce risk factors like obesity, high blood pressure, and cholesterol.
- Chronic Disease Management: Managing chronic conditions requires a coordinated approach that includes regular medical check-ups, medication adherence, and patient education. Programs that support lifestyle modifications and self-care are essential in controlling the progression of diseases.
- Policy and Regulation: Governments play a crucial role in reducing NCDs through policies such as taxing sugary drinks, banning tobacco advertising, and regulating trans fats. Strong legislation can create environments that promote healthier choices and reduce the risk factors associated with NCDs.
4. Infectious Disease Outbreak Preparedness and Response
Effective public health management involves preparedness for emerging infectious diseases, pandemics, and other health crises. Preparedness includes:
- Pandemic Planning: Health systems must have contingency plans in place for responding to large-scale outbreaks. This includes stockpiling medical supplies, training healthcare workers, and coordinating across sectors to minimize the impact of pandemics.
- Rapid Response Teams: Deploying trained public health professionals and healthcare workers in outbreak hotspots is crucial to containing diseases quickly. Their roles include case investigation, contact tracing, and community engagement.
- Global Collaboration: Public health agencies must collaborate internationally to share data, resources, and expertise. The World Health Organization (WHO) plays a vital role in coordinating global efforts to prevent and control infectious diseases.
5. Public Health Policy and Advocacy
A strong public health policy framework is necessary for effective disease prevention and control. Policies that support universal healthcare access, vaccination mandates, and environmental protections are essential. Public health advocates work to ensure that policies prioritize the well-being of populations, particularly vulnerable groups.
6. Technological Advances in Disease Prevention and Control
Modern technology has enhanced the ability of public health systems to prevent and control diseases. Innovations include:
- Data Analytics: Big data analytics allows for real-time disease surveillance and predictive modeling, enabling faster responses to outbreaks and better resource allocation.
- Telemedicine: Providing remote healthcare services through telemedicine helps in managing chronic diseases, especially in remote or underserved areas. It also reduces the strain on healthcare systems during pandemics.
- Genomics and Vaccines: Advances in genomics have led to the development of more effective vaccines and treatments tailored to specific diseases. For example, mRNA vaccines have been game-changers in the fight against COVID-19.
7. Community Engagement in Disease Prevention
Successful public health initiatives require community involvement. Public health professionals must engage with local populations, understand cultural contexts, and build trust to ensure the success of disease prevention programs. Community health workers play a key role in delivering healthcare services, promoting health education, and improving access to care.
8. Environmental and Social Determinants of Health

Public health management recognizes that environmental and social factors—such as clean water, air quality, housing conditions, education, and income—significantly influence disease prevention. Addressing these determinants is vital in preventing diseases at the population level.
Conclusion
Disease prevention and control are fundamental pillars of public health management, requiring a multifaceted approach that includes surveillance, vaccination, health education, policy advocacy, and community engagement. By addressing both communicable and non-communicable diseases, public health systems can reduce disease burden, prevent future outbreaks, and ensure healthier populations.
